Earlier this year, a review article was published covering the topic of carbohydrate restriction for diabetes with a distinct focus on type-1 diabetes, making this paper unique compared to other reviews that focus mostly on carbohydrate restriction for type-2 diabetes. In this paper the authors describe the history of dietary recommendations for diabetes, evidence in support of carbohydrate restriction, and address the major concerns associated with these types of diets. In this blog post we provide a brief overview of the important points of this review article.
Setting the stage
Carbohydrates come in many forms, but they are ultimately broken down into individual glucose molecules in the body. As glucose enters the bloodstream, the pancreas releases insulin to shuttle glucose out of our blood and into our cells. This is how we maintain healthy blood sugar levels since high blood sugar can be toxic and potentially damaging to blood vessels. If blood sugar gets too low, sirens go off to tell the liver to start releasing its stored glucose (liver glycogen) to bring blood sugar levels back up to normal.
This elegantly designed system is malfunctioning in diabetics, but in different ways depending on the type of diabetes.
Type 1 diabetes (T1D) is an autoimmune disorder where the pancreas fails to produce enough insulin. Managing T1D requires one to inject insulin themselves.
Type 2 diabetes (T2D) is a chronic disorder where the pancreas still maintains its function in producing insulin; only our cells no longer respond appropriately to its actions. As a result, blood sugar and insulin levels are elevated and, at this point, require intervention due to the harmful effects of chronically elevated blood sugar and insulin levels.
For a person with diabetes, achieving blood sugar control is the primary goal of any medical nutrition therapy, while also maintaining healthy blood lipid levels and ensuring normal growth and development in the case of children.
So, the primary goals are to:
1. Achieve healthy blood sugar levels
2. Achieve healthy blood lipid levels
In recent years, more recognition has been given to the relationship between post-meal (postprandial) high blood sugar (hyperglycemia) and elevated average blood sugar levels (HbA1c). In other words, meal by meal, how the food we eat affects our blood sugar levels dictate HbA1c levels – the marker both diabetics and healthy individuals alike are trying to normalize (often this means lowering). This means that controlling post-meal blood sugar spikes is a crucial variable to control.
Since carbohydrates are the most potent dietary factor affecting blood sugar levels, it makes sense that manipulating their intake may confer improved blood sugar control. Research has demonstrated that reducing carbohydrates can decrease post-meal blood sugar and insulin requirements better than any other dietary strategy, while also keeping other health markers in check (cardiometabolic risk factors). Moreover, the reduction of insulin and glucose-lowering medications will greatly reduce the costs associated with diabetes. Despite this, resistance against low-carb diets prevails due to concern for low blood sugar (hypoglycemia), ketoacidosis, nutrient deficiencies, stunted growth in children, and adherence. The remainder of this article will take a deep dive into the history of dietary recommendations for diabetes and address whether these concerns mentioned are worth advising against a low carbohydrate diet.
What did people with diabetes do before insulin?
As mentioned before, this paper focuses mostly on type-1 diabetes, which again requires administering insulin since type-1 diabetes cannot produce insulin themselves. Before the advent of insulin, carbohydrate restriction was the first line of care to prolong the lives of people with diabetes. Different dietary strategies were used throughout the centuries leading up to the discovery of insulin. Still, all included some degree of carbohydrate restriction via direct reduction of carbohydrates, fasting, or low-calorie diets restricting all macronutrients. Prolonged fasting and chronic caloric restriction are met with apparent concerns and dangerous side effects, such as extreme weight loss, ketoacidosis, undernutrition, and lean mass loss. However, further experimentation found that increasing dietary fat could preserve bodyweight and prevent these severe side effects, thus realizing a higher fat low-carb diet was better tolerated, and that some degree of ketosis was beneficial for diabetics.
Things changed in 1921 when insulin was discovered.
Diabetes management following the discovery of insulin
The decades following the discovery of insulin was progressively met by the increase in dietary carbohydrates. Blood sugar was rarely tested, and if it was, it was often in the fasted state. So, the impact of carbohydrates on postprandial blood sugar was going unnoticed. At this stage in time, the difference between nutritional ketosis and ketoacidosis was not appreciated, either. Practitioners thought it was more important to reduce ketones in the urine than glucose and actually preferred their patients have higher levels of the latter to lower the risk of ketosis and hypoglycemic events.
At the same time, dietary and blood cholesterol were being deemed dangerous for cardiovascular health, fueling the argument for lower fat, higher carbohydrate diets for diabetics. The idea was that if insulin could keep blood sugar under control, then diabetics could follow the diets recommended to the general population. These recommendations were in spite of evidence showing higher insulin requirements on high carbohydrate vs low carbohydrate diets, while higher carbohydrate diets were linked to elevated triglycerides in diabetics, and animal studies showed metabolic benefits to carbohydrate restriction.
The American Diabetes Association (ADA) published their first dietary guidelines in 1971, suggesting that 45% of energy intake from carbohydrates was acceptable. Approaching the 1980s, a low-fat, high-carbohydrate diet was advocated for weight control and chronic disease prevention to the general public. Simultaneously, diabetes research began increasingly focusing on the quality of carbohydrates in the diet, recommending high carbohydrate diets rich in fiber and limited in saturated fat. According to the ADA, total fat intake was to be kept below 30% of energy intake and carbohydrates of up to 55-60% of total calories.
In the 1990s, things changed when evidence from the Diabetes Control and Complications Trial (DCCT) showed that achieving near-normal glycemic control reduces the risk of microvascular complications. This trial demonstrated the changes in insulin dosages for variations in diet and encouraged the ADA to replace their distinct carbohydrate intake guidelines with the recommendation to focus on the quality of their diet (consideration for glycemic index* and fiber). Throughout the early 2000s, the ADA recommended against going below the recommended daily allowance (RDA) of 130g/day of carbohydrates, as carbohydrate-containing foods provided energy, fiber, vitamins, and minerals, despite no diabetes-related data was available to support these recommendations. From 2014 and onward, the ADA guidelines do not state any explicit recommendation for carbohydrate, protein, or fat intake. However, they have acknowledged that low carbohydrate diets may improve blood sugar control and lipid outcomes in type-2 diabetics. Generally speaking, though, large establishments continue to caution against low carbohydrate diets.
*Glycemic index: A tool that ranks foods on a scale from 1 to 100 based on their effect on blood sugar levels.
Appropriate insulin dosing is difficult
Today, diabetics self-monitor their blood sugar levels and adjust their premeal insulin doses to carbohydrate intake, as appropriate. This requires a patient to have a solid understanding of nutrition and accurately estimate the carbohydrate content in food, which studies show is extraordinarily challenging. Not to mention the different forms of insulin, impact of carbohydrate quality, the mismatch in carbohydrate absorption and effect of insulin, the impact of other macronutrients consumed alongside carbohydrates, the order in which food is eaten, stress, exercise, and other diet-unrelated factors. Due to these complexities, appropriate insulin dosing is incredibly difficult and requires extensive awareness and attention.
Macronutrients and blood sugar
Dietary carbohydrates are the primary determinant of blood sugar levels following a meal and insulin requirements. They are the only macronutrient that is directly converted to glucose. Protein influences blood sugar levels and insulin requirements due to gluconeogenic amino acids (amino acids that can be converted to glucose) and by triggering the release of the hormone glucagon, which tells the liver to produce glucose. However, the influence of protein is minor when compared to carbohydrates. Dietary fat slows the digestion of meals and can cause a shift in blood sugar rise to later. Even with careful control, the rise in blood sugar in response to a high-carbohydrate meal varies considerably among individuals. Preventing high- and low blood sugar (hyper- and hypoglycemia) in response to high-carbohydrate meals is a major challenge for diabetics. Continuous glucose monitors (CGMs) and insulin pumps provide diabetics with more flexibility and convenience for managing their diabetes, and their use has resulted in reduced HbA1c levels. Despite this, it still stands that in the US, diabetics are not achieving optimal glycemic control.
Current statistics show:
• According to the Type-1 Diabetes Exchange Registry, only 17% of children and 20% of adults achieve the HbA1c targets of <7.5% and 7%, respectively
• In recent years, glycemic control in adolescents is declining despite technological advancements
• Type-2 diabetics rarely achieve optimal glycemic and metabolic health risk markers
• Cardiovascular mortality and all-cause mortality are significantly higher in diabetics than in the general public
Where does a low-carb diet fit into all of this?
Recall that dietary carbohydrates have the most substantial influence of all macronutrients on our blood sugar and insulin levels.
Processed carbohydrates (e.g., refined grains) and simple sugars are digested rapidly and require immediate insulin. However, because the actions of insulin aren’t always quick, the timing and dosing of insulin are difficult for these foods. Besides, these foods are associated with increase cardiometabolic diabetes complications, which are made worse by increased insulin requirements. Thus, not aligning with the goals of any nutritional diabetes management strategy (1. blood sugar control, 2. healthy blood lipids). Type-2 diabetes and related disorders (e.g., metabolic syndrome) are characterized by insulin resistance and high insulin levels (hyperinsulinemia). The latter is also a typical feature of type-1 diabetes, as the way insulin is delivered exogenously requires higher whole-body concentrations to control the liver’s glucose output to prevent hyperglycemia. This can lead to increased weight gain due to insulin’s actions on our body fat stores, increasing the risk of metabolic syndrome in type-1 diabetics. So, even though intensive insulin treatments on a high carbohydrate diet can reduce glucose spikes, it increases the risk of fat gain and increased caloric intake from having to manage frequent low blood sugar (responding to low blood sugar by eating something with high sugar content) with the additional problems associated with hyperinsulinemia. Altogether, the solution to these issues is to focus on the quality of carbohydrates consumed (low glycemic index/glycemic load) or reduce total dietary carbohydrates.
Let’s look at that first factor: the quality of carbohydrate.
Not all types of carbohydrates behave similarly. Foods high in fiber slow carbohydrate absorption and may also improve insulin sensitivity through their actions on the gut microbiome. Although high-fiber diets are associated with improved outcomes in both type-1 and type-2 diabetics, it’s hard to know for certain its direct contribution due to confounding factors and interpretations of the data. Nonetheless, research does suggest fiber may provide benefits for glycemic control.
An additional qualitative aspect of carbohydrates is their glycemic index (GI) and glycemic load** (GL). Low-GI/GL diets have shown to provide small benefits to diabetics for blood sugar control and are also associated with reduced insulin requirements, improved quality of life, reduced lipids, and weight loss. Ultimately, the lower the GI/GL of a food and the higher the fiber, the better it comes to managing blood sugar.
**Glycemic load: GI multiplied by the amount of digestible carbohydrate consumed.
Now, let`s look at the second factor: the amount of carbohydrate.
If you are familiar with ketogenic metabolism, you will know that humans have no essential need for dietary carbohydrates, like they do proteins and fats. Some may think of type-2 diabetes as “impaired carbohydrate intolerance.” As diabetes researcher Jonathon Little explained in an interview: “If you have lactose intolerance, you remove lactose. If you have gluten intolerance, you remove gluten. So, if you have carbohydrate intolerance, maybe you should remove carbohydrates.”
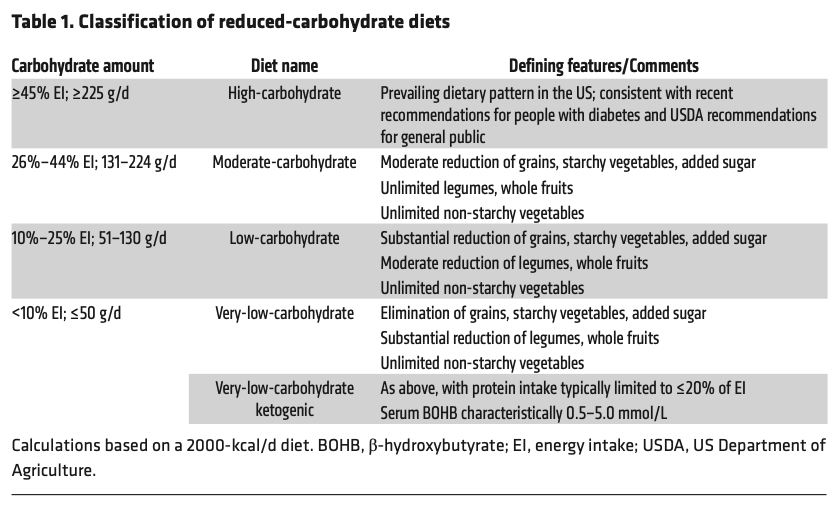
The amount of carbohydrates in a diet can be categorized as high-carbohydrate (>45% of energy intake) and reduced-carbohydrate (<45% of energy intake). The latter is further broken down depending on the degree of carbohydrate restriction, as per table 1 below:
A ketogenic diet is the only version of a carbohydrate-restricted diet defined by a specific biomarker – ketones. With a significant reduction in carbohydrates (<30-50 grams per day), insulin is relatively suppressed, and its opposing hormone, glucagon, increases. This high glucagon to insulin ratio tells our fat cells to release stored fat and the liver to start producing ketones from this fat. Nutritional ketosis is defined by blood ketone levels within the range of 0.5-3.0 mmol/L, which is in stark contrast to diabetic ketoacidosis (uncontrolled ketone production), where ketones exceed 5 mmol/L.
Does carbohydrate reduction work for type-1 diabetes?
Truthfully, rigorous research on carbohydrate restriction for type-1 diabetes is limited. However, the authors conducted a systematic search to gather evidence from studies using carbohydrate-restricted diets (<45% of energy intake for at least 2-months). They assessed the results from 24 studies (4 randomized controlled trials (RCT), 5 uncontrolled interventional studies, 3 observational studies, and 12 case reports or series). They found that only those studies using low- and very-low-carb diets reported mean HbA1c levels of less than 7.5%, and that except for one case report, in the studies of very-low-carbohydrate diets, HbA1c was in the normal range and insulin requirements were low. Despite limitations, there is widespread interest in carbohydrate restriction for diabetes management, and due to these promising preliminary results, we suspect more research will be dedicated to addressing this topic.
Results from 316 people with type-1 diabetes following a very-low-carb diet for at least 3 months showed mean HbA1c levels at 5.67%, daily insulin dosages at 0.4 U/kg/day, and mean CGM blood sugar levels at 104 mg/dL with a mean, standard deviation of 36 mg/dL. In the short-term RCTs, low carb and very-low-carb diets reduced HbA1c, insulin doses, glycemic variability, and time spent in hypoglycemia compared to high-carb diets. Blood lipid values between individuals are variable; generally, there is an improvement in triglycerides and HDL-cholesterol, but several case reports show an elevation in LDL-cholesterol.
Looking to evidence from low carbohydrate diets in type-2 diabetes
Though different, type-1 and type-2 diabetes share common features and comorbidities, and studies of carbohydrate restriction in type-2 diabetes can be informative for type-1s. Meta-analyses of trials using carbohydrate restriction in type-2 diabetes show only a small lowering in HbA1c, but do show reduced usage of glucose-lowering medications and improved triglycerides and HDL-cholesterol (LDL-cholesterol results are inconsistent). Many reports also show benefits independent of weight loss suggesting benefits inherent to carbohydrate restriction itself. There are several limitations to studying dietary interventions over the long-term, especially ones that may not be familiar to the participants. In a nonrandomized trial with intense individual support (web-based resources, tracking tools, telemedicine support), a ketogenic diet proved sustainable and effective in 262 adults with type-2 diabetes, with 74% of participants still following the diet at the 2-year mark. This trial showed a mean weight loss of 11.9 kg, a mean HbA1c reduction of 0.9%, and over 50% reduction in glucose-lowering medications, (except for metformin). Most importantly, over 50% of participants achieved HbA1c levels below 6.5%, categorizing them as “diabetes reversal.”
Safety concerns for type-1 diabetics
The paper provides the major barriers preventing widespread clinical acceptance of carbohydrate restriction for type-1 diabetes. Acknowledging the validity of these concerns, they are summarized below.
1. Hypoglycemia
Due to the reduction in insulin requirements that accompany a very-low-carb diet and removing the difficulties of appropriate insulin dosing, this way of eating may actually lower the risk of hypoglycemic events. Results from two RCTs reported less time spent in hypoglycemia with carbohydrate restriction, compared to high-carb diets. Reports from an online community reported infrequent or reduced severe hypoglycemia after adopting a very-low-carb diet, compared to their previous diet. It is also the case that in a state of nutritional ketosis, ketone bodies protect the brain from the potentially damaging effects of hypoglycemia due to their role as an alternative fuel; however, this has not been studied in the context of diabetics.
2. Ketoacidosis
The risk of ketoacidosis in type-1 diabetics following a very-low-carb diet is a valid concern since insulin inhibits “runaway ketone” (aka ketoacidosis) but type-1 diabetics do not produce insulin. However, the difference between nutritional ketosis (physiological) and ketoacidosis (pathological) must be appreciated to understand why the risks associated with very-low-carb diets are not well-founded. Ketoacidosis results from complete insulin-deficiency, and the amount of insulin that type-1 diabetics administer even on a very-low-carb diet is almost always sufficient to suppress ketoacidosis. The authors suggest that due to the well-managed and stabilized blood sugar levels on a very-low-carb diet, patients can use small increases in blood sugar as a warning sign that they might need more insulin to prevent unwanted consequences (e.g., uncontrolled increase in ketones). Ketoacidosis is rarely reported in the available literature on carbohydrate restriction in type-1 diabetics. There is a possibility for ketoacidosis with blood sugar levels below 250 mg/dL; however, this has not been described in the context of type-1 diabetics on a very-low-carb diet.
3. Cardiovascular disease risk
Carbohydrate-restricted diets predictably improve triglycerides and HDL-cholesterol. However, the effects on LDL-cholesterol are less predictable and may be influenced by the types of fats consumed. While speculative, the improvements in triglycerides and HDL-cholesterol may offset the possible adverse effects of elevated LDL. Furthermore, the increase in LDL may be due to a rise in the less-atherogenic LDL particles (large buoyant, as compared to small dense). Most importantly, HbA1c has been identified as the strongest predictor of cardiovascular events in diabetics. So, this should be the priority of any dietary management strategy.
4. Nutrient insufficiency
A very-low-carb diet can be optimally formulated to cover all nutritional needs. Nutrient-dense foods, such as animal foods, nuts, seeds, non-starchy vegetables, and limited amounts of low-sugar fruits can be included with this way of eating.
5. Growth
Stunted growth has been reported with the traditional ketogenic diet in children with refractory epilepsy; however, this diet is extremely restricted in carbohydrates and protein, differing substantially from that used in type-1 diabetes. Nonetheless, there have been reports of children with type-1 diabetes experiencing delayed growth, but the effects may be due to other confounding factors. The authors note that more research is needed to address this concern.
6. Other concerns
Of the practical concerns, restrictive diets, and therefore increased risk of eating disorders, and adherence are the major issues. Studies employing carbohydrate restriction in diabetics are often met with low long-term adherence, despite successful results.
Bottom Line
Carbohydrate restriction has been used throughout history for managing diabetes, but was largely replaced with the discovery of insulin and villainizing of dietary fat. Preliminary evidence suggests that very-low-carbohydrate diets need to be reconsidered in future research for their therapeutic advantages and ability to manage glycemia in both type-1 and type-2 diabetics effectively. Achieving optimal glycemic control should be the priority when considering optimal macronutrient ratios due to the strong evidence to suggest this factor’s influence on severe diabetes complications.
We look forward to future research addressing the utility of this dietary strategy and the long-term safety of these diets.
Written by: Kristi Storoschuk; Edited by: Dominic DAgostino, Csilla Ari Dagostino