By now, you are likely in the know of how important insulin sensitivity is to our overall metabolic health and longevity. Insulin resistance essentially precedes type-2 diabetes, and is tightly linked with obesity and metabolic inflexibility. Metabolic inflexibility is thought to contribute to the development of not only obesity and type-2 diabetes, but also cardiovascular disease, chronic inflammation, reduced immune function, and an increased risk for certain cancers.
Humans have evolved to withstand periods of food abundance and scarcity, and it is our inherent metabolic flexibility that permits our survival without food. Metabolic flexibility is our body’s ability to efficiently adapt our metabolism to different energy sources depending on demand and availability to maintain energy homeostasis. In simplest terms, it is our cell’s capacity to switch between burning glucose and fat with ease.
The issue we are seeing today is that the majority of people are stuck in this glucose-dominant state, where overnutrition or caloric excess, combined with a sedentary lifestyle, causes us to lose our metabolic flexibility over time. This topic is very important as the loss of metabolic flexibility is a hallmark of many chronic metabolic diseases, as mentioned previously, but is likely something that can be quickly restored through lifestyle change.
It was 1999 when Kelley et al. discovered that lean individuals could easily adapt their metabolism to the fasting state or insulin infusion compared to obese individuals. Put another way, lean individuals displayed a level of metabolic flexibility that obese individuals lacked. A healthy metabolism will switch to burning fat while fasting, and effectively shut it off when nutrients (or certain hormones, e.g., insulin) are present. In this study, the obese participants did not effectively make this switch to burning fat while fasting, nor was it reduced following insulin infusion, compared to the lean participants.
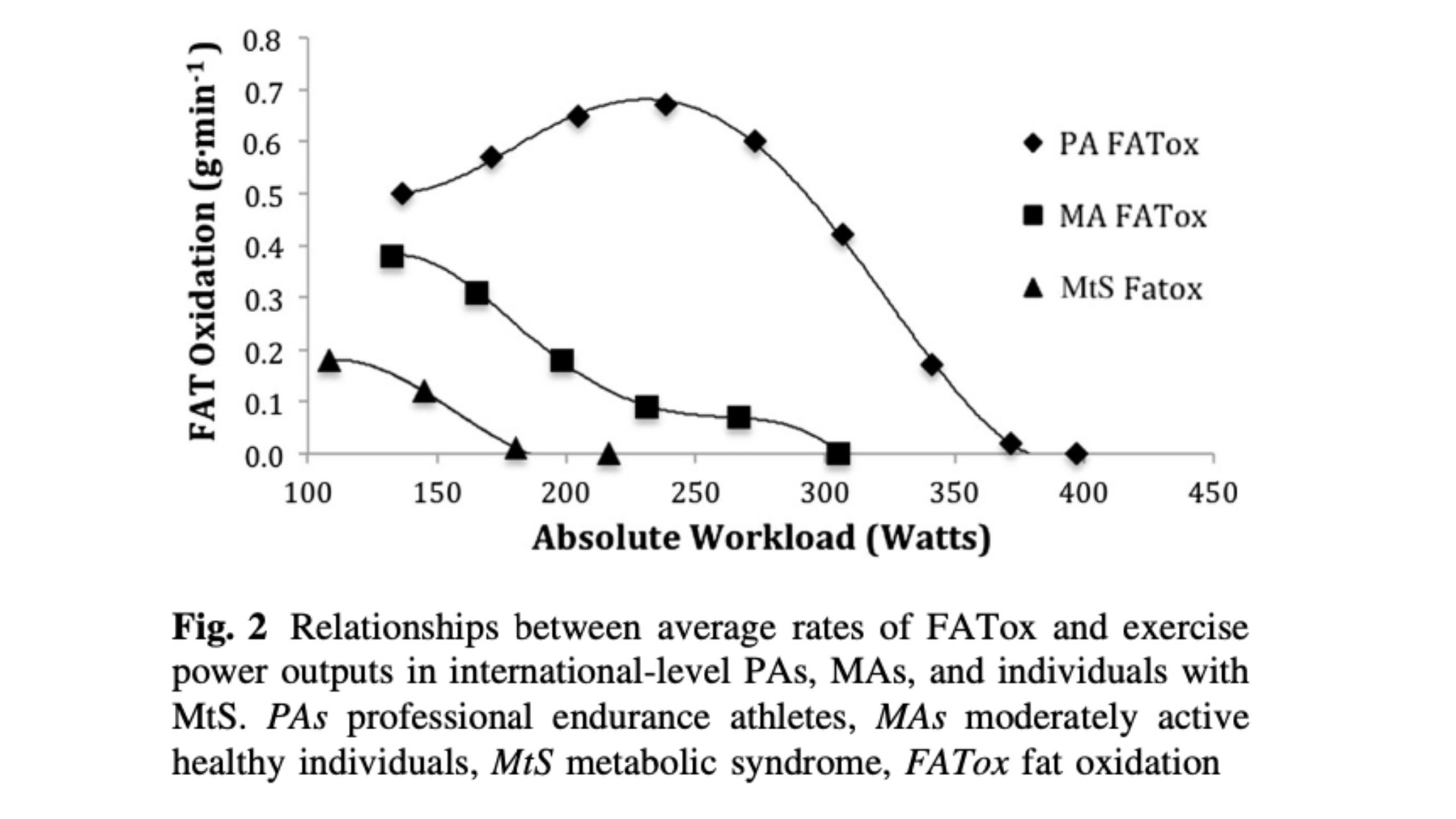
It is now generally understood that metabolic flexibility is linked to our metabolic health, as elegantly shown by San-Millan and Brooks where individuals with metabolic syndrome showed impaired metabolic flexibility during an incremental exercise test, compared to recreationally active and elite athlete participants with superb metabolic flexibility. The participants with metabolic inflexibility were burning significantly more glucose at rest and low intensity exercise. The theory is that their mitochondria weren’t functioning properly, therefore unable to burn fat efficiently. As a consequence, glucose is burned outside of the mitochondria (in the cytosol), generating lactate in the process.
Speaking of mitochondria…
Mitochondria are at the helm of our metabolism and are often referred to as the powerhouse of the cell; the energy plant where energy from the food we eat or stored on our body is converted to cellular energy. The capacity of our mitochondria to adapt to different fuel sources is essentially what defines metabolic flexibility on a cellular level, and thus mitochondrial function is at the core of this discussion.
On a whole-body level, metabolic flexibility involves proper nutrient sensing responses, uptake, transport, and storage of nutrients, and appropriately burning these nutrients as fuel. This entire system acts in response to the timing and frequency of meals (or intermittent fasting), meal composition (protein, carbs, and fat), exercise, temperature (e.g., cold exposure), and is influenced by numerous hormones.
When we eat a meal containing carbohydrates, insulin is secreted from the pancreas into the bloodstream, and the release of insulin’s opposing hormone, glucagon, is suppressed. A high insulin to glucagon ratio favors glucose metabolism, and reduces the mobilization of fat. While fasting, insulin secretion slows, and glucagon eventually takes precedence, lowering the insulin to glucagon ratio, and causing the body to reduce glucose uptake and mobilize fat for fuel. If you fast long enough, glucagon will also promote the breakdown of stored glycogen and the production of ketones in the liver. Enhanced fat oxidation and glycogenolysis is further augmented by an increase in catecholamines, which may be why we feel more awake as we transition from a fed to fasted state.
This low insulin to glucagon ratio is essential to maintaining metabolic flexibility, and likely mitochondrial health as well. This is supported by the evidence whereby chronic caloric excess (and therefore increased insulin to glucagon ratio) overwhelms the mitochondria and leads to inappropriate fuel utilization, storage of nutrients, and an increase in oxidative stress. At a molecular level, a high NADH/NAD+ ratio may inhibit the expression of genes important for mitochondrial function. Moreover, prolonged elevated insulin levels and therefore reduced fat burning is associated with a buildup of intramuscular triglycerides (IMTG) that, over time, will ultimately impair insulin signalling. This is likely why in the original study by Kelley et al., obese individuals couldn’t make that metabolic switch to fat burning while fasting, because they had lost the capacity to do so. The takeaway here is that chronically eating in a caloric surplus impedes metabolic flexibility and promotes insulin resistance, and paints a picture for how obesity can lead to insulin resistance.
When it comes to the relationship between insulin resistance and metabolic flexibility, the main driver is the level of adiposity and the amount of skeletal muscle mass. Skeletal muscle size and function is so important for metabolic flexibility because this organ accounts for the very large majority of glucose disposal, and therefore plays a starring role in glycemic control and insulin sensitivity. It has been suggested that skeletal muscle mitochondrial dysfunction precedes insulin resistance, as mitochondrial adaptations in the skeletal muscle of type-2 diabetics do not respond to exercise as they should (by increasing mtDNA replication), in addition to displaying reduced mitochondrial function.
If you’re concerned about your metabolic flexibility and want to restore or improve it… here’s what you can do:
EXERCISE! (it’s the biggest lever we can pull)
Without a shadow of a doubt, a sedentary lifestyle year after year will do a major disservice to your metabolic flexibility. Whether you’re running, cycling, lifting weights, or simply working around the yard, regular exercise will help you to improve mitochondrial function and metabolic flexibility. Exercise increases the activation of AMPK, an important nutrient sensor involved in increasing mitochondrial quality and quantity through the expression of several transcription factors and co-activators. Through several complex pathways, mitochondria respond to exercise by replicating, growing, and building a stronger mitochondrial network (mitochondrial biogenesis). Combined with a caloric deficit (further increases AMPK), and thus weight loss, regular exercise has been shown to improve insulin sensitivity, mitochondrial content, and metabolic flexibility in both normal and overweight participants. In addition, exercise stimulates insulin-independent glucose uptake, meaning glucose can enter your cells without the help of insulin (a major advantage!). If you simply go for a 10-15 min walk after eating a meal (especially if it’s carbs) you will reduce the postprandial glucose spike and insulin secretion, which simultaneously stimulates glycogen replenishment and fat oxidation. The take home message is that exercise is the surest way to get those mitochondria firing, promote glucose disposal, insulin sensitivity, and improve metabolic flexibility.
But you can also eat less, lose weight, and/or fast!
As highlighted already, being overweight and frequent feedings impedes metabolic flexibility. In contrast, eating in a caloric deficit helps the body breakdown stored fat in places we don’t want it stored (visceral fat) which is likely very important for restoring obesity-related metabolic inflexibility. In the study mentioned previously by Kelley et al., weight loss in previously obese participants improved insulin sensitivity and their response to insulin infusion, indicating improved metabolic flexibility.
Going extended periods without eating at all, as you would with intermittent fasting or prolonged fasting, allows the body to enter periods of low insulin and high glucagon, forcing the mitochondria of our cells to maximize fat oxidation.. Intermittent fasting can be something you practice daily (e.g., 16/8 time-restricted feeding) or periodic multi-day fasts (e.g., 48-72 hour fasts). If you are starting at a place of poor metabolic flexibility, you may find it difficult to fast, and it is recommended that you start slow (~10-12-hour fasts) and work your way up to longer fasts.
How caloric restriction and intermittent fasting may work to improve metabolic flexibility is intuitively easy to understand. If we stop eating, we essentially force the body to burn its stored energy through lowering insulin and elevating glucagon. Since we only store minimal amounts of glucose as glycogen (relative to how much fat we can store), glucose can only sustain us for so long until we need to make the switch to fat. The resulting cascade of cellular events (e.g. activated AMPK, enhanced mitochondrial activity) ensures we have energy needs met, although the rate of transition may vary considerably between individuals.
Can you improve metabolic flexibility by removing carbohydrates from the diet independent of caloric intake or weight loss? Maybe!
We certainly need more research to help clarify because most studies using carbohydrate-restriction for improving disorders associated with metabolic inflexibility are often confounded by simply producing a calorie deficit (ie. subjects lost weight), so it’s hard to tease the two apart. That said, athletes who follow ketogenic diets show significantly greater capacity to burn fat, which is likely part of “training” the metabolism to use fat as fuel. Also, a study in obese men found significantly increased fat oxidation relative to glucose after a short term ketogenic diet, compared to an isocaloric balanced diet. Since a ketogenic diet mimics the fasting state in a lot of ways, it is very possible that periodic ketosis induced by a ketogenic diet can be used to improve metabolic flexibility on the fat-burning end of the spectrum. The increased fat oxidation is likely driven by the suppression of insulin signaling associated with a ketogenic diet. The potential caveat is that it may come at the cost of reduced capacity to burn glucose (e.g., suppressed insulin reduces PDH activity) if one sustains carb restriction for long periods of time. Whether that is an issue is not well-known, nor does it matter if you are using a ketogenic diet to manage a disease process, like epilepsy. However, by definition, metabolic flexibility is the ability to switch back and forth between glucose and fat, so if you are following a ketogenic diet for general wellness, periodically kicking yourself out of ketosis may actually be of benefit in terms of metabolic flexibility. The simple solution could be to simply couple a lower carb diet (like 100g/day) with time restricted feeding. Introducing small amounts of carbs in occasionally and keeping your body “hungry” for carbs (ie. keeping low fasting glucose levels) may allow you to increase insulin sensitivity while also enhancing carb tolerable and metabolic flexibility.
In summary, if the goal is to be as metabolically flexible and insulin sensitive as you can be, you want to have a high tolerance for carbohydrates, while also being a very efficient fat-burner. And it’s very unlikely that you will achieve this by eating all the time, being overweight, and not exercising. Depending upon personal preferences each individual will need to adjust dietary patterns, fasting and exercise selection to fit their lifestyle, but when these things are combined together that will maximize your metabolic flexibility.
Written by: Kristi Storoschuk, edited by: Dr. Dominic D`Agostino