
A new paper, published in the American Journal of Lifestyle Medicine by a group at Harvard Medical School and Harvard School of Dental Medicine, reports on the results of a pilot program using Continuous Glucose Monitors (CGMs) as part of a Metabolic Immersion program.
After being trained in the responsible use of CGMs and being screened for underlying health conditions, a group of 13 healthy Harvard Medical and Dental students were provided with CGMs for between 30 and 40 days. Over this time, they also tracked dietary intake, engaged in journal clubs, and interacted with patients in hospital settings as part of their normal medical school curriculum and training. At the beginning and end of the study, the students completed questionnaires to see how their experience with CGMs impacted their personal behavior, nutrition choices, awareness of glucose metabolism, and overall medical education experience.
Students were so excited about the project that, within a week of the first student donning the first CGM, dozens of other students were asking to enroll. Ultimately, given the available resources, 40 students were able to acquire CGMs. A quantitative analysis of student response drawn from the completion survey confirms students had an overwhelmingly positive experience with this wearable technology.
100% agreed or strongly agreed with the statements:
- “Wearing a CGM gave me valuable insights into my own body’s reactions to foods”
- “Wearing a CGM was an experience that was valuable to my medical education”
- “Wearing a CGM was an experience that will help me better serve patients with diabetes in future”
- “Future students should be provided with the opportunity to wear CGMs”
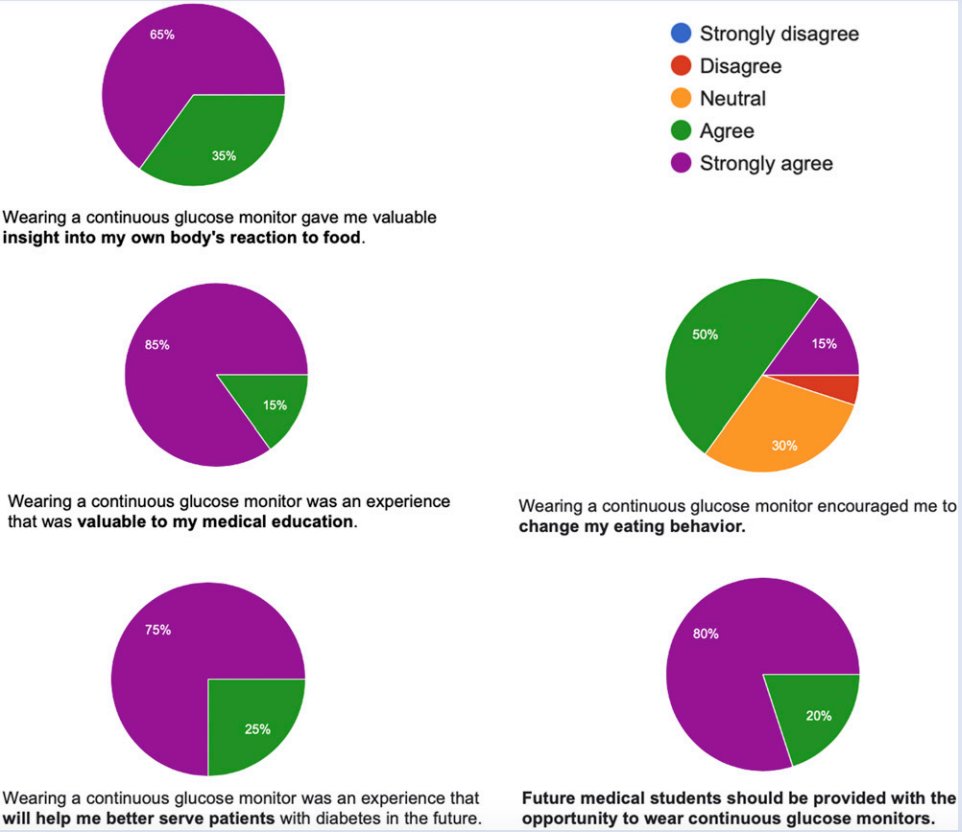
Figure 1.
Additionally, two-thirds of students reported that wearing a CGM encouraged them to change their own eating behaviors. In the qualitative reporting, some students reported improved physical and mental performance when they avoided high-glycemic carbohydrates and, thus, reduced glycemic excursions, and many reported feeling more cognizant and mindful of what they were consuming.
Students also reported becoming “metabolically woke” with respect to the quality (or lack thereof) of diet and nutrition advice provided to patients. Quoting from the paper, “Students reported that dietary advice provided to patients is typically “crude,” “cookie-cutter,” “surface level,” “inadequate,” and “prescriptive and not individualized,” and that current standard of advice focused on energy balance and “calories in – calories out” is “oversimplified” and “misleading,” for patients. No students reported satisfaction for the state of nutrition in healthcare in regards to education and training.” The use of CGMs as a behavioral tool may provide an informative feedback loop to improve eating behaviors, glycemic control, and ultimately sustained weight loss and associated metabolic biomarkers (eg. HbA1C, Insulin, etc.). It is possible that the resulting increase in CGM-associated nutritional awareness in this pilot study may be a game changer for the use of this wearable technology in future nutritional education.
While exciting, this project is also provocative. Not all physicians are supportive of medical students receiving CGM, and many are concerned that providing CGM to “healthy users” will lead to over-pathologizing high glycemic variations. Fortunately, this pilot project included responsible training about data interpretation to address this concern. Additionally, rather than stealing CGMs away from patients who need them, these students were being transformed into patient advocates in real-time. Their newfound expertise with CGMs provided an immersive education on the wearable technology (and associated App) to help understand and advocate for enhanced awareness and management of diabetes.
Often times, when medical professionals prescribe these types of medical devices and recommend other nutritional/lifestyle modifications, patients still leave the office with questions. There are many aspects of using CGMs (eg. placement, App difficulties, meal timing) that, left unclear, would lead to less than optimal glycemic management. Therefore, the more medical professionals utilize these devices and master them from a human behavioral perspective, the more they are able to help their patients succeed. Medical students in the study reported feeling more personal control (accountability) of their own health after undergoing proper CGM training and use, and with the same training, diabetics will be more confident in leveraging and discussing this technology for better diabetes management and long term outcomes. It should be the goal of all health care providers to use every means possible to empower their patients, and to build upon the doctor-patient relationship. The doctor-patient team capable of honing the benefits of the CGM can provide another level and care and management for improved long term outcomes.
With the early use of CGM in medical students, it also serves as an immersive experience to learn more about nutrition and lifestyle modification in a way that does not replace, but compliments, other crucial parts of the medical curriculum. It is an unfortunate reality that many medical students and residents eventually lose sight of their own health due to the long work hours, stress of training, and poor food choices, but CGMs may allow students and residents to improve their own health and serve as better role models for their patients.
While this pilot was small in scale and only recently released, the positive response within the Harvard system and beyond has set the stage for future similar projects, potentially involving other medical schools and professionals at other levels of training, including residents and perhaps attending doctors. Furthermore, with more support from the medical community, younger generations aspiring to optimize their health may feel more comfortable talking about nutrition to their healthcare providers and exploring the benefits of CGMs and other emerging wearable technologies.
While I realize many of you might not be medical professionals or have aspirations to attending medical school, the reason I find this particularly uplifting and exciting is because it could mark a catalytic change in the culture of medicine from one that leans away from metabolic health to one that leans into it. For further breakdown of the study, please take 16 minutes to watch this video by study Harvard Medical Student Nick Norwitz: https://youtu.be/YwKr2kQwGxk
By: Francis “Sean” Walson (USF Morsani College of Medicine M.D. Candidate, Class of 2024), Natalya Thomas (USF; Judy Genshaft Honors College) and Dr. Dominic D’Agostino
