
The current treatment protocol for type 2 diabetic patients admitted to the hospital largely ignores the more current and progressive understanding of the underlying pathological process that leads to the development of the disease. Current management does not consider recent advances in metabolic research regarding the control of type 2 diabetes mellitus (DM2) and blood glucose including the ketogenic diet (KD) or time restricted feeding (TRF).
There is an abundance of evidence regarding the ketogenic diet (KD) and time restricted feeding (TRF) relating to the effectiveness of treating and even reversing type 2 diabetes mellitus (DM2). Multiple clinical trials and various studies have demonstrated that patients are able to significantly reduce and even eliminate the need for exogenous insulin therapy after only a short time following a KD or TRF protocol (Abbasi, 2018; Feinman et al., 2015; Furmli et al. 2018). While the literature usually addresses the ability of the KD to control DM2 from a community health or primary care perspective, it is not often discussed as a potential strategy for acute care settings. However, according to recent advances in metabolic research, considering the KD as a treatment option for these patients is a major opportunity for the medical establishment to improve patient outcomes.
Current Treatment of DM2
Upon hospital admission of a diabetic patient, much of the dietary and nutritional strategies to control or reverse DM2 are largely ignored. The extent of nutritional therapy typically ends with a physician order for an often subjective “carb controlled diet.” This is typically misunderstood or ignored by patients and even by nursing professionals that are under immense pressure to preserve patient satisfaction . (What better way to make a patient happy than to feed them whatever they want?) DM2 patients often have their metformin discontinued and they are placed on an insulin sliding scale. Based on the acute, immediate needs of the patient, this may be necessary. However, the healthcare professionals should view this protocol only as the minimum requirement to acutely stabilize a patient or maintain patient safety. This management is far from providing comprehensive, holistic patient treatment and care. Additionally, continuing to feed a diabetic patient carbohydrates and controlling their blood glucose with exogenous insulin, only perpetuates the process of the disease.
The Conventional Metabolic Perspective of DM2
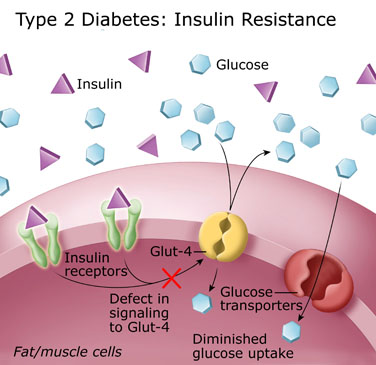
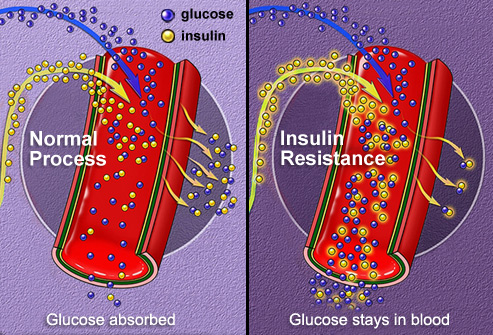
It is generally understood among the public that DM2 is a “sugar disease” that results in chronically elevated blood glucose levels. The scientific foundation for the development of this state is multifactorial, but DM2 has been thought to be the result of developed insulin resistance in combination with other metabolic factors [metabolic syndrome]. The belief is that years of carbohydrate rich food choices cause spikes in blood glucose producing a compensatory insulin response necessary to prevent hyperglycemia. The continual secretion of insulin induces resistance by the cells (most abundantly in skeletal muscles) thereby initiating a dangerous cycle requiring increasing amounts of insulin to be secreted in order to produce the same reduction in blood glucose levels. This generates a hyperinsulinemic effect that masks the clinical expression of DM2, but leads to the eventual dysfunction of pancreatic beta-cells responsible for secreting insulin (McCance & Huether, 2014). The beta cell is extremely sensitive to high levels of blood glucose, therefore, carb rich dietary choices that lead to the perpetual secretion of insulin eventually lead to beta-cell dysfunction and the clinical development of DM2.
Once the administration of oral medication options are no longer effective, the patient is placed on exogenous insulin to maintain safe blood glucose levels. However, this only forces more glucose into the cell inducing worsening metabolic disease and does nothing to address the root cause. The common understanding is that the cells have developed insulin insensitivity and now require exogenous insulin to facilitate glucose transport into the cell.
Progressive research challenges this understanding as many hypothesize that the prevention of glucose from entering the cell is not due to cell insensitivity, but rather from intracellular signaling that inhibits glucose import.
The New Paradigm/ From the Metabolic Perspective
What if the cause of DM2 was not necessarily the cell becoming resistant to insulin, but rather the cell just becoming too full of glucose that it begins to hinder further transport of glucose into the cell? What if our cells just needed to be cleaned out of their glucose? Dr. Peter Attia and nephrologist Dr. Jason Fung (2019) elaborate on this concept on Dr. Attia’s recent podcast The Drive. Considering the success demonstrated by the KD and TRF to not only control blood glucose, but to significantly decrease the need for diabetic medications including insulin, it may be more likely that the foundational basis of DM2 is tied to the state of hyperinsulinemia rather than the preconceived notion of insulin insensitivity (Abbasi, 2018; Feinman et al., 2015; Furmli et al. 2018). Therefore, the implementation of these therapies should at least be considered upon hospital admission for all DM2 patients. Using a KD and TRF protocol may finally begin to treat patients in a way that addresses some of the foundational causes for the development of DM2 at a cellular and metabolic level.
From the Patient Care Perspective
The above proposed treatment and therapy options should be considered for several reasons. First, people are admitted to the hospital because their condition is acute and severe. These patients are at highest risk for the complications and comorbidities related to DM2, therefore, it is evident that their current treatment regimen is inadequate necessitating additional therapy, and likely, an entirely different approach. Secondly, in hospital settings, patients are monitored more closely which would prevent or significantly reduce the chance of complications, such as hypoglycemia. Lastly, the time spent in the hospital provides an opportunity for more complete and extensive educational sessions by professionals qualified to teach these protocols. Starting people on the KD diet and/or on a TRF protocol allows modifications to be made, questions to be answered in real time, and provides a safe environment for patients during this transition. The extensive education implemented during the admission may sustain better adherence to the KD and TRF protocol after discharge, thus enhancing the beneficial effects.
Time to Evolve
Medicine and nursing science is predicated on practices that are evidence-based. While this ensures progress that is rooted in science with evidence and credibility, it also causes progress at an exceptionally slow pace. The laborious process in search of consensus is holding back the evolution of treatment modalities that could significantly improve patient outcomes. In the case of DM2, long-term therapy can start in hospitals, upon admission. It is time for healthcare to utilize some of the progressive approaches to therapy that have been demonstrating significant promise with very little risk. The current management perpetuates the status quo; a continued and growing pandemic with prolific consequences. Healthcare professionals must shift the treatment paradigm and begin implementing innovative and progressive treatment options that have the potential to help millions of patients suffering with DM2.
Written by: Vin Petronelli; Edited by: Dr. Dominic D`Agostino
REFERENCES
Abbasi, J. (2018). Interest in the ketogenic diet grows for weight loss and type 2 diabetes. Jama, 319(3), 215-217. doi:10.1001/jama.2017.20639
Feinman, R. D., Pogozelski, W. K., Astrup, A., Bernstein, R. K., Fine, E. J., Westman, E. C., … Worm, N. (2015). Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base. Nutrition, 31(1), 1–13. https://doi-org.chamberlainuniversity.idm.oclc.org/10.1016/j.nut.2014.06.011
Furmli, S., Elmasry, R., Ramos, M., & Fung, J. (2018). Therapeutic use of intermittent fasting for people with type 2 diabetes as an alternative to insulin. BMJ case reports, 2018, bcr2017221854. doi:10.1136/bcr-2017-221854
Leal, J., Gray, A.M., & Clarke, P.M. (2008). Development of life-expectancy tables for people with type 2 diabetes. European Heart Journal, 30 (7), 834-838. Doi: 10.1093/eurheartj/ehn567
McCance, K. L., Huether, S. E., Brashers, V. L., & Rote, N. S. (2018). Pathophysiology: the biologic basis for disease in adults and children. St. Louis, MO: Elsevier.
Mootha, V. (2004). Err and Gabpa/b specify PGC-1 -dependent oxidative phosphorylation gene expression that is altered in diabetic muscle. Proceedings of the National Academy of Sciences, 10(17), 6570–6575. doi: 10.1073/pnas.0505194102
Dr. Peter Attia. (Producer). (2019, June 24). The Drive #59. Jason Fung: Fasting as a potent antidote to obesity, insulin resistance, type 2 diabetes and the many symptoms of metabolic illness. [Audio Podcast}
Panel, M., Ghaleh, B., & Morin, D. (n.d.). (2018) Mitochondria and aging: A role for the mitochondrial transition pore? Aging Cell, 17(4). https://doi-org.chamberlainuniversity.idm.oclc.org/10.1111/acel.12793
Stubbs, B. J., Cox, P. J., Evans, R. D., Santer, P., Miller, J. J., Faull, O. K., … Clarke, K. (2017). On the Metabolism of Exogenous Ketones in Humans. Frontiers in Physiology, 8, 848. https://doi-org.chamberlainuniversity.idm.oclc.org/10.3389/fphys.2017.00848
