 Despite Alzheimer’s Disease (AD) being discovered over a century ago, there is still no effective treatment available today. In fact, the rates are only growing and AD has become the most common form of cognitive impairment as we age. This has a lot of people thinking… if treatments aren’t currently effective, how can we prevent this disease?
Despite Alzheimer’s Disease (AD) being discovered over a century ago, there is still no effective treatment available today. In fact, the rates are only growing and AD has become the most common form of cognitive impairment as we age. This has a lot of people thinking… if treatments aren’t currently effective, how can we prevent this disease?
Prevention of any disease is tricky, because that requires us to understand the fundamentals of the cause. The cause of AD is still a bit of a mystery, but we do know there is an increased risk in Type-2 diabetics, individuals carrying 1 or 2 APOE4 alleles, and sedentary individuals, among others. Most of which can be approached by lifestyle interventions, today’s most promising form of AD prevention.
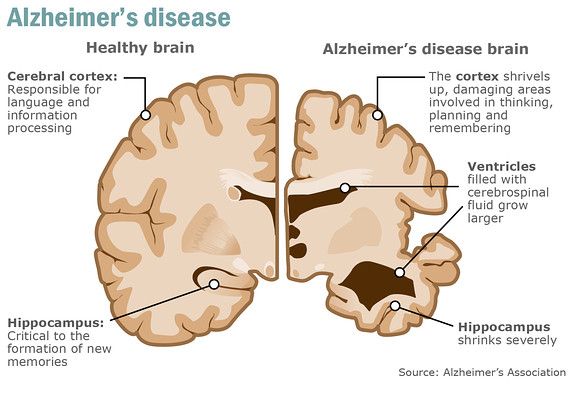
An Important Hallmark of AD
While there is a growing body of literature addressing one of the common hallmarks of AD: the impaired brain energy metabolism, which we believe deserves significantly more attention. The human brain accounts for ~2% of our total body weight yet consumes up to 25% of our energy requirements (Cunnane, et al., 2016). In other words, the brain has very high energy demands. If the brain isn’t receiving adequate fuel, cognitive decline can manifest and it is now well understood that brain glucose uptake and metabolism is impaired in the AD brain. This ultimately is perceived as an energy crisis in the brain where there simply is not enough fuel to build, repair, and maintain a healthy brain. The concept of lower blood glucose utilization in the brain as an early sign of AD progression was introduced in the late 1980’s by Hoyer et al. and is essentially hypoglycemia of the brain (Hoyer, et al., 1988). Unfortunately, there is a vicious cycle that occurs in the development of AD whereby the brain cannot adequately use glucose as fuel, leading to less energy production in the brain which can result in neuronal death and deteriorating neurotransmission, manifesting in cognitive decline, and further reduction in brain glucose uptake. It is hypothesized that the lack of energy flow to the brain could be contributing to the deteriorating neuronal function and development of AD, rather than this being a consequence of the disease.
Ketones to Bypass Impaired Brain Glucose Metabolism
Glucose is the predominant fuel for the brain, but cannot supply adequate fuel to the AD brain, putting the brain at risk for starvation and exhaustion. However, when ketones become available, the brain will preferentially take up and utilize them as fuel, even in the presence of glucose. What’s more is that brain uptake of ketones is in direct proportion to their plasma concentration, whereas glucose enters in response to the brain’s energy demands. We know that the brain loves ketones, this has been demonstrated on various occasions, such as in Dr. Stephen Cunnane’s research. In fact, it was demonstrated much earlier (1967) in a study of a 40-day starvation period, ketones were supplying two thirds of the brain’s energy requirements. This was the first study to show that ketones are an alternative fuel source to glucose.
We know that brain glucose metabolism is impaired in AD, but ketone bodies appear to have no issue entering the brain and being metabolized as fuel. What if this impaired brain glucose uptake was taking place early in life and that it was contributing the development of AD? Bypassing this impairment and maintaining the brain fuel supply could be an incredible strategy to prevent or delay the onset of AD. Could ketones fill this gap?
In 1981, it was demonstrated that in AD, brain glucose uptake decreased by 26%, but brain ketone uptake remained normal (Lying-Tunell U, et al., 1981). Another group later showed a decrease in brain glucose utilization of 45% in individuals with perceived early stages of AD (Hoyer et al., 1988). Ketone production and utilization does not appear to be impaired with age, as studies have shown similar levels of both production and utilization in young and aged individuals (Freemantle et al., 2009).
It was identified using labelled AcAc PET tracer that ketone uptake and metabolism remains intact even in early AD (Castellano, et al., 2015). Specifically, this study confirmed a decrease in brain glucose uptake and identified no difference in ketone uptake between the early AD individuals and age-matched controls. This same study confirmed that brain ketone utilization in AD is positively correlated to plasma ketone levels, which were shown to be the same in control and AD participants, supporting the rationale behind using ketones to overcome the energy deficit of the deteriorating brain.
A Promising Case Report
A very encouraging case report on the use of ketogenic therapies in AD was published by Mary Newport and colleagues (Newport et al., 2014). The report addressed a 63-year-old male, APOE4-positive with younger-onset, sporadic AD, beginning from the age of 51 when he began experiencing noticeable short-term memory loss. By 2006 he was displaying the telling signs of AD, unable to carry out activities of daily living. From 2004 to 2008 his Mini-Mental State Examination (MMSE) dropped 12 points and an MRI revealed brain atrophy. In 2008, he began consuming 165mL of a 4:3 mixture of MCT to coconut oil in 3-4 servings over a course of the day. By day 75 of this treatment, his MMSE score improved from 12 to 20. MRI scans revealed no change from 2008 to 2010, suggesting his disease was not progressing. In 2010, he was administered three 28.7g servings of R-3-hydroxyl R-3-hydroxybutyrate ketone monoester (KME) daily. Within DAYS the patient regained the ability to complete activities without assistance, write out the alphabet, and dress himself among other tasks. He even reported for himself improved mood and more energy. These treatments were all given in combination with a normal diet. It was noted that his improved cognition and physical activity levels were greatest with peak plasma ketone concentrations (6-8 mmol/L). What’s more is that over the course of this 2-year treatment investigation, no adverse side-effects were reported.
The science is constantly adding pieces to the puzzle and we remain hopeful for the future of prevention and reversal of cognitive decline, especially in regards to the role of ketones. Not to mention that metabolic derangement appears to be associated with various other neurological disorders, whereby ketones may offer a potential therapy for.
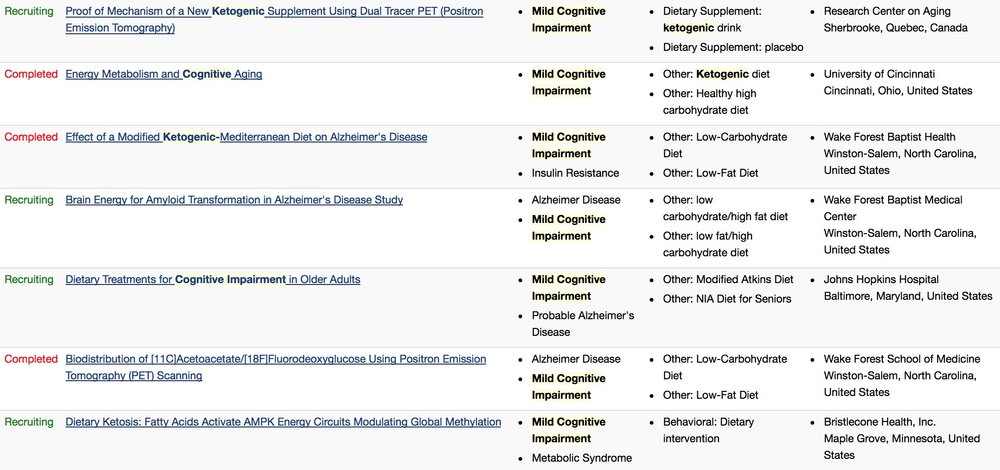
Current Clinical Trials for Ketogenic Therapies for Cognitive Impairment (as per clinicaltrials.gov)
Cunnane SC, et al. 2016. Can ketones compensate for deteriorating brain glucose uptake during aging? Implications for the risk and treatment of Alzheimer’s disease. Ann NY Acad Sci. 1367:12-20.
Hoyer S, et al. 1988. Glucose metabolism as the site of the primary abnormality in early onset dementia of Alzheimer type? J Neurol. 235: 143– 148.
Courchesne-Loyer A, et al. 2017. Inverse relationship between brain glucose and ketone metabolism in adults during short-term moderate dietary ketosis: A dual tracer quantitative positron emission tomography study. J Cereb Blood Flow Metab. 37(7):2485–2493.
Lying-Tunell U et al. 1981. Cerebral blood flow and metabolic rate of oxygen, glucose, lactate, pyruvate, ketone bodies and amino acids. Acta Neurol Scand. 63: 337–350
Freemantle E. et al. 2009. Metabolic response to a ketogenic breakfast in the healthy elderly. J Nutr Health Aging 13: 293–298.
Castellano CA, et al. 2015. Lower brain 18F-fluorodeoxyglucose uptake but normal 11C-acetoacetate metabolism in mild Alzheimer’s disease dementia. J Alzheimers Dis. 43(4):1343-1353.
Newport MT, VanItallie TB, Kashiwaya Y, King MT, Veech RL. A new way to produce hyperketonemia: use of ketone ester in a case of Alzheimer’s disease. Alzheimers Dement. 2014;11(1):99-103.
Written by: Kristi Storoschuk; Edited by: Dr. Dominic DAgostino