Image credit: Nutrients 2019, 11(4), 811; https://doi.org/10.3390/nu11040811
Migraine is not simply a “bad headache”, it is a in fact a neurological disorder and can be extremely debilitating, ultimately affecting quality of life. Despite the commonality of migraine, there are no current treatment options that either do the job or are absent of unwanted side-effects. It is not fully understood what causes migraines; however, there is plenty of sound speculation around it.
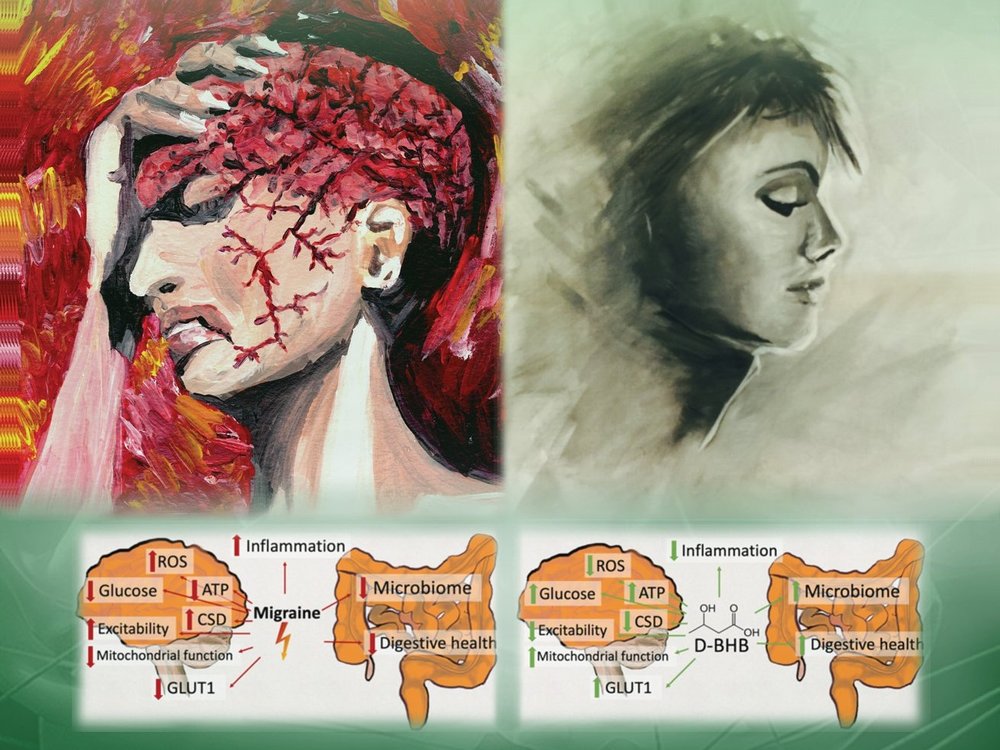
There is an increasing amount of evidence suggesting migraine is a response to brain energy deficiency or oxidative stress levels that exceed antioxidant capacity. The ketogenic diet, a diet mimicking fasting that leads to the elevation of ketone bodies, is a therapeutic intervention targeting brain metabolism that has recently shown great promise in the prevention of migraine. Ketone bodies are an alternative fuel source for the brain and are hence likely able to circumvent some of the abnormalities in glucose metabolism and transport found in migraine. Recent research has also demonstrated the signalling roles of ketone bodies, in particular beta-hydroxybutyrate, with the potential to benefit other pathways believed to be underpinning migraine.
Recap on ketones, ketosis, and the ketogenic diet
Ketone bodies serve as an alternative fuel source to the brain, along with almost all other tissues. They are the by-products of fat metabolism, produced from our stored body fat (eg. fasting) or the fat we eat (eg. ketogenic diet), after we’ve burned through our liver glycogen stores and glucose is no longer readily available.
Within the last few decades, the ketogenic diet and ketones themselves have been gaining a lot of attention for their therapeutic applications in a variety of neurological disorders. This is largely due to the association with impaired brain glucose metabolism and ketones ability to bypass these issues and overcome the accompanied energy deficit. The most well-studied ketone body is beta-hydroxybutyrate (BHB), since this is the primary ketone body produced in a state of ketosis (accounts for up to 70% of all ketone bodies produced) [1].
Two reasons BHB is of interest as an alternative fuel source to the brain:
1. It doesn’t require a glucose transporter protein to get inside the cell
2. It acts as a signalling molecule (ie. can communicate with other parts of the cell and body)
The average person following a standard diet will likely never raise their blood ketone levels above 0.2 mmol/L unless they partake in prolonged fasts. Those following a ketogenic diet and/or periodically fast will likely see an elevation between 0.5-5 mmol/L, which is considered a state of ketosis (ie. you have effectively switched from burning primarily glucose for fuel to free fatty acids and ketones).
Research with ketones for migraines
There are several case reports showing the potential for ketosis to protect against migraine. In one study, the ketogenic diet resulted in up to an 80% reduction in migraine frequency, severity and use of medication in 96 migraine patients [2]. An additional study found the ketogenic diet reduced migraine days by 62.5% in 18 patients that experience episodic migraines [3]. It’s even been suggested that the benefits of ketosis on migraines could outlast the time spent in ketosis. This is sometimes the case with epilepsy where seizures do not return even after coming off a ketogenic diet.
Common features of migraine
· Abnormal glucose metabolism and transport
· Mitochondrial dysfunction
· Oxidative stress
· Cerebral excitability
· Inflammation
· Abnormalities in the gut microbiome
How ketones may target all features of migraine
Glucose Metabolism
Hypoglycemia is associated with migraine and it is commonly reported that fasting or skipping meals can trigger migraine. Ketones very easily overcome inadequate brain glucose availability/metabolism and therefore restore the brain’s large energy demands. What’s more is that ketone metabolism vs glucose metabolism at the cellular level generates more energy in the form of ATP per oxygen molecule consumed, in other words ketones give you a better bang for your buck! This additionally aids in the energy deficit experienced when glucose metabolism is impaired or glucose supply is low.
Insulin resistance has also been linked to migraine. Insulin in regard to the topic at hand, essentially works hand in hand with these glucose transport proteins to shuttle glucose into our cells from the blood. So, when we are insulin resistant and therefore can’t effectively respond to insulin, the brain cannot receive adequate amounts of glucose.
Mitochondrial Function
There is quite a bit of evidence linking mitochondrial function to migraine. For example, there is a higher prevalence of migraines in individuals with mitochondrial disorders [4], as well as a more common maternal transmission of migraine [5]. This highlights the possibility that mitochondrial DNA (mtDNA), which is derived exclusively from the mother, could be involved. There have even been findings showing a genetic link between mitochondrial function and migraine and a reduction of mitochondrial enzymes in migraine, further supporting the link between mitochondrial function in migraine.
Ketone bodies routinely demonstrate beneficial effects on mitochondria and are commonly referred to as a “clean” energy source. In animal models, ketosis has even shown to promote the generation of new mitochondria (aka mitochondrial biogenesis).
Oxidative Stress
The generation of reactive oxygen species (ROS) and reactive nitrogen species (RNS) are natural by products of metabolism and play vital roles in the body. Problems arise, however, when their levels surpass the antioxidant capacity of the cell, therefore promoting oxidative stress and impacting both mitochondrial function and energy metabolism. There are many lines of evidence to suggest that migraine is associated with reduced anti-oxidant capacity and/or increased oxidative stress.
Ketone bodies, in particular BHB, have antioxidant potential through reduced production of ROS as well as their ability to scavenge free radicals [6]. In addition, BHB works on the level of our epigenome promoting the expression of genes that help combat oxidative stress. It is therefore suggested that BHB may be a strategy to combat the oxidative stress associated with migraine.
In short: ketones reduce oxidative stress by producing less ROS, scavenging free radicals, and upregulating pathways that manage oxidative stress.
Excitability of the Brain
Brain excitability is governed by two primary neurotransmitters: GABA and glutamate. GABA is our calming neurotransmitter, while glutamate is our excitatory. An imbalance of the two, whereby glutamate dominates, can cause over stimulation and neuronal hyperexcitability. This is very likely linked to migraine due to its overlap with epilepsy, including the possible underlying mechanisms and shared pharmacological agents used to treat both conditions.
Ketone bodies promote a higher GABA to glutamate ratio, thereby reducing neuronal firing and calming the brain [7]. Ketone bodies appear to inhibit glutamate transport in addition to reducing glutamate release, as well as other contributing factors. This reduction in excitability could therefore offer protection against migraine.
In short: ketones reduce hyperexcitability in the brain by increasing the GABA to glutamate ratio and reducing neuronal firing.
Inflammation
There are certainly several lines of evidence to suggest migraine is associated with neuroinflammation, despite not being considered an inflammatory disease. Studies have shown various pro-inflammatory molecules present in migraine. Ketone bodies are repeatedly described as being anti-inflammatory, particularly after the 2015 paper by Youm et al. reporting on BHB’s ability to inhibit the activation of the NLRP3 inflammasome [8]. The reduction in oxidative stress is another way in which BHB prevents inflammation. The anti-inflammatory effects of BHB could be a way to dampen the potential inflammation underpinning migraine.
In short: ketones reduce/prevent inflammation by inhibiting the activation of inflammatory pathways, as well as their ability to reduce oxidative stress.
Gut Microbiome
More and more research is linking the health of our gut to our overall health and there is reason to believe the gut microbiome is playing a role in the pathophysiology of migraine. This is supported by the increased frequency of gastrointestinal (GI) symptoms or disorders commonly reported in migraine patients [9]. A well-formulated ketogenic diet and nutritional ketosis may alter the gut microbiome in a way that improves gut permeability, production of neuropeptides, and inflammation of the GI-tract, therefore presenting themselves as a potential therapy.
In short: ketones and the ketogenic diet may alter the gut microbiome in a way that improves the health of our gut and associated conditions.
Conclusion
It is clear that there are many players underlying the cause of migraine, and that these players are likely not shared in each individual. Ketone bodies are notorious for their systemic effects on the body and their use a multifaceted therapy in a range of diseases and disorders. Ketone bodies have the potential to exploit not one, but all the potential contributors to migraine described in this article. In this way, ketones could be a broad range therapy for all migraine individuals, independent of etiology.
This is certainly a new area of research and for the most part, speculative. However, there is currently a registered controlled trial investigating the potential preventative anti-migraine effects of BHB supplementation without dietary restriction which will help us understand whether it is the carbohydrate restriction, dietary composition, or ketones themselves that offer migraine relief.
Ketosis, whether induced by diet or supplementation, is safe, well-tolerated, and is rarely associated with negative side-effects. What’s more is that all of the factors described in this article have been linked to various other neurological and metabolic conditions. So, ketones could be preventing more than just those pesky migraines.
Written by: Kristi Storoschuk; Edited by: Dr. Dominic DAgostino
References:
- Dedkova, E.N.; Blatter, L.A. Role of β-hydroxybutyrate, its polymer poly-β-hydroxybutyrate and inorganic polyphosphate in mammalian health and disease. Front. Physiol. 2014, 5, 260.
- Di Lorenzo, C.; Coppola, G.; Sirianni, G.; Di Lorenzo, G.; Bracaglia, M.; Di Lenola, D.; Siracusano, A.; Rossi, P.; Pierelli, F. Migraine improvement during short lasting ketogenesis: A proof-of-concept study. Eur. J. Neurol. 2015, 22, 170–177.
- Di Lorenzo, C.; Coppola, G.; Bracaglia, M.; Di Lenola, D.; Evangelista, M.; Sirianni, G.; Rossi, P.; Di Lorenzo, G.; Serrao, M.; Parisi, V.; et al. Cortical functional correlates of responsiveness to short-lasting preventive intervention with ketogenic diet in migraine: A multimodal evoked potentials study. J. Headache Pain 2016, 17, 58.
- Kraya, T.; Deschauer, M.; Joshi, P.R.; Zierz, S.; Gaul, C. Prevalence of Headache in Patients With Mitochondrial Disease: A Cross-Sectional Study. Headache 2018, 58, 45–52.
- Lemos, C.; Alonso, I.; Barros, J.; Sequeiros, J.; Pereira-Monteiro, J.; Mendonça, D.; Sousa, A. Assessing risk factors for migraine: Differences in gender transmission. PLoS ONE 2012, 7, e50626.
- Haces,M.L.;Hernández-Fonseca,K.;Medina-Campos,O.N.;Montiel,T.;Pedraza-Chaverri,J.;Massieu,L. Antioxidant capacity contributes to protection of ketone bodies against oxidative damage induced during hypoglycemic conditions. Exp. Neurol. 2008, 211, 85–96.
- Ma,W.;Berg,J.; Yellen,G.KetogenicdietmetabolitesreducefiringincentralneuronsbyopeningK(ATP)channels. J. Neurosci. 2007, 27, 3618–3625.
- Youm, Y.-H.; Nguyen, K.Y.; Grant, R.W.; Goldberg, E.L.; Bodogai, M.; Kim, D.; D’Agostino, D.;Planavsky, N.; Lupfer, C.; Kanneganti, T.D.; et al. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat. Med. 2015, 21, 263–269.
- Cámara-Lemarroy,C.R.;Rodriguez-Gutierrez,R.;Monreal-Robles,R.;Marfil-Rivera,A. Gastrointestinal disorders associated with migraine: A comprehensive review. World J. Gastroenterol. 2016, 22, 8149–8160.